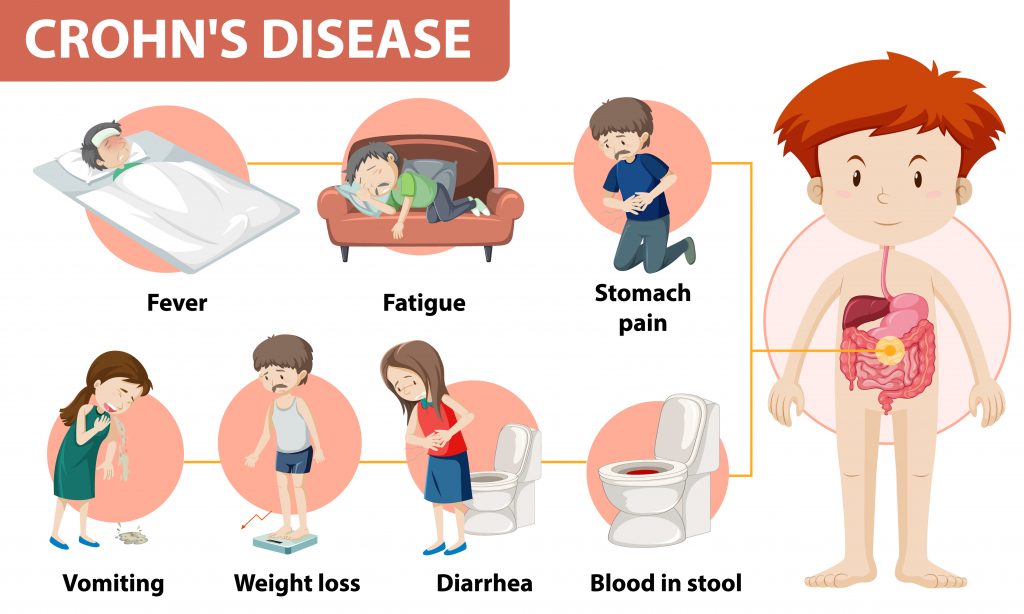
You many wonder what exactly is Crohn’s Disease and why fatigue is part of the illness. Many people with the two primary types of inflammatory bowel disease (IBD), Crohn’s disease and ulcerative colitis, experience fatigue. Fatigue typically causes exhaustion and weariness that is not always relieved after a night’s rest or a nap. It can take a serious toll on a person’s quality of life.
What is Crohn’s Disease
Crohn’s disease and ulcerative colitis are separate conditions, but both cause chronic inflammation in the digestive tract. While Crohn’s disease can lead to inflammation in any part of the gastrointestinal system between the mouth and the anus, ulcerative colitis only causes inflammation in the innermost lining of the colon.
Besides the direct effects of IBD, other factors linked to ulcerative colitis and Crohn’s disease — including pain, stress, or sleep disruption — can also contribute to fatigue. Fatigue is a tricky problem that may not always have an easy answer. If you’re experiencing Crohn’s- or colitis-related fatigue, your first step should be to bring it up with your treatment team. This way, you can work together to identify what’s causing it and apply an effective solution.
Sobriety can improve the symptoms of IBD
Addiction recovery research indicates that alcohol and smoking can exacerbate symptoms in people who have Crohn’s and colitis, prompting flare-ups in some situations and medication absorption challenges in others. People who stop consuming alcohol or quit smoking may find that their IBD symptoms improve.
In addition, some people living with Crohn’s or colitis may take narcotics to deal with the pain that the conditions cause. Researchers believe that use of narcotics for pain relief in IBD is related to a longer duration of the disease and an increase in mental health challenges.
People in recovery who have IBD should talk with their treatment teams to ensure that they have access to methods of controlling pain that won’t prompt a relapse in substance abuse.
Controlling IBD
Many people living with Crohn’s disease or ulcerative colitis find that their fatigue levels drop as their IBD symptoms subside. Research indicates that the body’s response to inflammation, both in the gastrointestinal tract or elsewhere, may cause fatigue.
People living with Crohn’s disease and ulcerative colitis may be dealing with a host of symptoms that can worsen fatigue. For instance, constipation and IBD can impact your quality of life and make it more challenging to stick with your normal routines, leading to the possibility of fatigue.
People whose diseases are in remission may have fewer complaints of fatigue. To help manage your Crohn’s- and colitis-related fatigue:
● Take your medications as they are prescribed by your doctor.
● Make sure you’re getting an adequate amount of iron in your diet. Anemia is a common complication of Crohn’s or colitis and being anemic can worsen fatigue.
Could your medication cause your fatigue
Certain medications used to treat IBD can directly cause fatigue, so you should talk to your doctor to see if one of your medications could be contributing to your symptoms. In addition, some drugs can interfere with sleep, contributing to or worsening fatigue.
Your treatment team can help you determine whether any of your medications are associated with fatigue — individually or in combination with the other medications you’re taking. Make sure to talk about any over-the-counter (OTC) drugs or supplements you’re taking as well. Discuss changing medication(s) or dosages if necessary.
Crohn’s Disease and nutrition
People with Crohn’s disease or ulcerative colitis may be at greater risk for nutrient deficiencies or malnutrition. This could be due to diarrhea, inadequate nutrient absorption related to gastrointestinal tract inflammation, or other causes. For instance, it’s particularly essential to get enough vitamins A, E, and K if you have IBD. These vitamins are important for cell production, preventing cell damage, fighting infections, and maintaining bone health.
Ask your doctor if you should consider getting bloodwork to check for any vitamin or mineral deficiencies. In many cases, a nutrient deficiency is easily rectified with a nutrient supplementation plan or a change in diet.
By addressing the root causes of your fatigue, you could be on your way to rectifying the issue and finding an increase in your energy levels.
By Nyaka Mwanza: Nyaka Mwanza is a freelance writer for MyHealthTeams. She completed a B.A. in Communications: Visual Media from American University and undertook post-baccalaureate studies in Health/Behavioral Communications and Marketing at Johns Hopkins University. Nyaka is a Zambian-born, E.U. citizen who was raised in sub-Saharan Africa and Jacksonville, N.C. However, she has called Washington, D.C., home for most of her life. For much of her career, Nyaka has worked with large global health nonprofits focused on improving health outcomes for women and children/
References
1. What Is IBD? — Crohn’s & Colitis Foundation
2. Constipation with IBD: Tips for Relief
3. Crohn’s disease symptom: Is fatigue common?