Substance Abuse and Mental Health Disorders How They Interact
In the realm of mental health, a complex interplay exists between substance abuse and various psychiatric disorders. This intricate relationship has garnered increasing attention in the United States as researchers, healthcare professionals, and policymakers strive to understand and address the underlying factors contributing to both substance abuse and mental health issues. Exploring this link unveils a multifaceted landscape that necessitates comprehensive approaches to prevention, intervention, and treatment.
Substance Abuse and Mental Health Disorders What Research Says
Substance abuse and mental health disorders often intertwine, creating a challenging scenario for individuals and society as a whole. According to the National Institute on Drug Abuse (NIDA), approximately half of those with a substance use disorder (SUD) also experience a co-occurring mental health disorder, and vice versa. This phenomenon, known as comorbidity, underscores the intricate relationship between substance abuse and mental health.
One of the primary drivers behind the connection between substance abuse and mental health disorders is self-medication. Many individuals struggling with psychiatric conditions such as depression, anxiety, or post-traumatic stress disorder (PTSD) may turn to drugs or alcohol as a means of alleviating their symptoms temporarily. However, while substance use might provide short-term relief, it often exacerbates underlying mental health issues in the long run, leading to a vicious cycle of dependency and worsening psychological distress.
Understanding the Interplay of Genetics and Environment
Moreover, genetic and environmental factors contribute significantly to the development of both substance abuse and mental health disorders. Genetic predispositions, trauma, socioeconomic status, and access to healthcare all play pivotal roles in shaping an individual’s susceptibility to these conditions. In the United States, health disparities, systemic inequalities, and inadequate access to mental healthcare exacerbate the prevalence of substance abuse and co-occurring mental health disorders, particularly among marginalized communities.
The impact of substance abuse on mental health cannot be overstated. Chronic drug or alcohol use can disrupt neurotransmitter systems in the brain, impair cognitive function, and alter mood regulation mechanisms, thereby exacerbating symptoms of psychiatric disorders. Conversely, individuals with untreated mental health conditions may resort to substance abuse as a coping mechanism, further complicating their clinical presentation and impeding recovery efforts.
Integrating Care for Co-Occurring Disorders
Addressing the intertwined nature of substance abuse and mental health disorders requires a holistic approach that integrates medical, psychological, and social interventions. Early identification and comprehensive assessment of co-occurring disorders are essential for guiding personalized treatment plans that address the unique needs of each individual. Integrated care models that coordinate mental health services with substance abuse treatment programs have shown promise in improving outcomes and reducing relapse rates.
Furthermore, destigmatizing mental illness and substance abuse is paramount to fostering a supportive environment where individuals feel empowered to seek help without fear of judgment or discrimination. Education campaigns, community outreach initiatives, and advocacy efforts play vital roles in raising awareness, challenging stereotypes, and promoting empathy and understanding.
In the United States, efforts to address the link between substance abuse and mental health disorders must also encompass broader systemic changes aimed at improving access to affordable healthcare, expanding mental health services, and implementing evidence-based prevention strategies. By investing in early intervention, comprehensive treatment, and recovery support services, we can mitigate the adverse effects of substance abuse and mental illness, enhance public health outcomes, and cultivate a more resilient and compassionate society.
Conclusion
In conclusion, the intricate relationship between substance abuse and mental health disorders underscores the need for a multifaceted approach that addresses biological, psychological, and social factors. By unraveling this link and implementing integrated interventions, we can promote healing, resilience, and recovery for individuals and communities across the United States.
Valley Vista in Vermont specializes in dual diagnosis therapy, integrating treatment for addiction and mental health disorders for holistic recovery. Contact us today to learn more about Comprehensive Dual Diagnosis Therapy.
More Articles To Read About Recovery
Breaking Free from Adderall Addiction
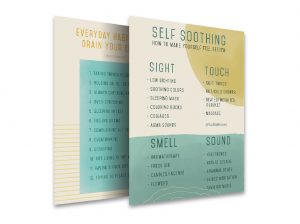
Mental And Physical Tips For Self-Care In Recovery
Supporting Loved Ones Through Challenges