Why Addiction Is Still a Leading Mental Health Crisis in 2025 — and What Recovery Communities Can Do Differently
In 2025, addiction remains deeply woven into the global mental health crisis. Despite advances in awareness and treatment, millions are still falling through the cracks — and too often, the systems built to help either aren’t equipped or aren’t reaching them. As someone who has been following addiction in America for over 20 years, this is disappointing at best. But, it is not hopeless and we need to share solutions.
What the Numbers Say About The Mental Health Crisis (and Why It Matters)
-
According to a 2025 report from World Health Organization (WHO), over 1 billion people worldwide are living with mental health conditions — including depression, anxiety, trauma-related disorders, and more. World Health Organization
-
In the U.S., the 2024 national survey by Substance Abuse and Mental Health Services Administration (SAMHSA) found that among adults with mental illness in the last year, a shocking 34.5% also had a substance use disorder (SUD). SAMHSA+1
-
Overall, roughly 48.5 million Americans (about 16.7%) experienced a SUD in the past year — underscoring that addiction affects tens of millions across demographics. American Addiction Centers
-
Even more alarming: many of those needing help never get it. In 2024, approximately 80% of people who needed treatment for substance use disorders did not receive it. SAMHSA+1
These statistics show addiction isn’t a “niche problem.” It’s a public-health crisis wrapped up in mental health, trauma, isolation, and systemic failure — still very much alive in 2025.
Why We’re Still Here: The Underlying Challenges Of A Mental Health Crisis
Co-occurring Disorders: Addiction & Mental Health
Addiction rarely stands alone. Most people struggling with substance use also carry mental-health burdens like anxiety, depression, PTSD, or past trauma. But standard treatment often treats addiction and mental health separately. That disjointed approach leaves many without the integrated support they truly need. SAMHSA+2ScienceDirect+2
Gaps in Treatment Access
Despite rising need, the gap between those who need treatment and those who receive it remains enormous. Barriers like cost, availability, stigma, and lack of integrated care prevent many from accessing help. Mental Health America+2NCDAS+2
Trauma, Stress & the Emotional Load
Many people enter addiction already carrying heavy trauma — emotional wounds, generational pain, unhealed grief, or disrupted attachment. Unless care systems address trauma, underlying pain drives relapse. Recent studies on trauma-informed care (TIC) show strong promise: clients in TIC-based addiction treatment programs have shown significant reductions in substance use, depression, anxiety, and PTSD symptoms over time. ScienceDirect+1
Isolation, Social Disconnection & Stigma
Addiction is still stigmatized. People often feel judged rather than supported. Isolation, shame, and fractured community ties make it much harder to seek help — and even harder to stay in recovery.
What Recovery Communities Must Do Differently — The Shift We Need Now
If we truly want to turn the tide in 2025 and beyond on the mental health crisis, recovery efforts must evolve. Here are the changes, backed by data and grounded in what healing actually looks like.
1. Embrace Trauma-Informed, Integrated Care
Rather than treating addiction and mental health separately, programs should:
-
Recognize the role past trauma plays.
-
Offer therapeutic support for both mental health and substance use — side by side.
-
Provide environments where people feel safe, heard, and validated.
When done right, trauma-informed residential treatment has shown dramatic improvements not just in abstinence but in emotional health and long-term well-being. ScienceDirect+1
2. Expand Access to Treatment & Reduce Barriers
We need to reach the 80%+ who need help but don’t get it. This means:
-
More affordable or sliding-scale treatment options
-
Telehealth, community-based services, and peer-led support
-
Outreach and education to reduce stigma
-
Policies that address mental-health workforce shortages and funding gaps
3. Build Community, Connection & Belonging
Recovery isn’t just about sobriety — it’s about connection. Communities of support, peer groups, family-friendly healing models, and inclusive spaces matter. When people feel seen, supported, and connected, recovery becomes sustainable.
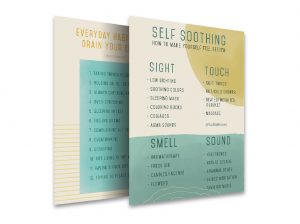
4. Offer Hope Through Education & Prevention
Prevention isn’t just for youth — it matters for adults too. Education around mental health, stress, trauma, healthy coping, and self-compassion reduces the risk of turning to substances. Recovery communities can lead that education with workshops, content, and outreach.
5. Advocate for Policy & Systemic Change
We need structural change: better insurance coverage, mental-health parity laws, accessible treatment funding, and policy support for integrated mental and addiction care. Recovery communities should use their voices to influence change — not just treat individuals.
Why It Matters — More Than Ever
In 2025, with global mental-health numbers surging, addiction isn’t quietly hiding. It’s intertwined with anxiety, trauma, depression, and social disconnection. Lives are being lost. Families are being torn apart. Generational pain is being passed down. We need to act to help with this mental health crisis.
But it doesn’t have to stay this way. With compassion, community, and care that meets the whole person — not just the substance use — we can shift this crisis trajectory.
Recovery isn’t just possible. With the right systems — trauma-informed, integrated, accessible — recovery can be life-changing.
And healing can ripple out into families and communities.
CHECK OUT MY FIRST BOOK
Follow us on Instagram
Like us on Facebook
Comment on our posts